Patient-Practitioner Relationship
- Investigate if doctors' dressing style is important.
- Wanted to see if there were demographic differences in the beliefs.
- 475 Participants from Scotland completed interviews after visiting the doctor.
- “Which doctor would you feel happiest about seeing for the first time?” Score from 0-5.
- Asked about confidence in the ability of the doctors.
- Asked if they would be unhappy consulting them.
- Asked which one looks most like your doctor.
- Asked closed questions about their dressing sense and attitudes to different clothes.
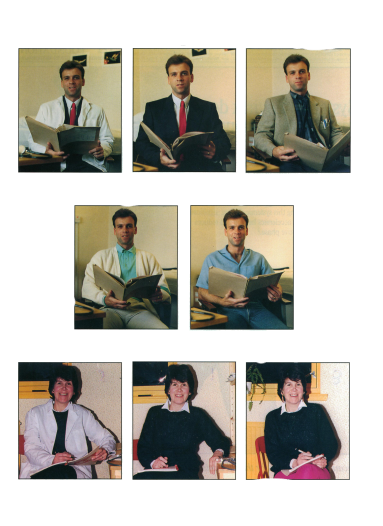
- 5 photos of men, 3 photos of women. Fewer photos of women since they had less distinct styles.
- Both models had the same pose for each photo. Results:
- Doctor in a smart suit was most popular.
- Tweed jacket and Tie – 2nd most popular.
- Jeans – Least popular.
- Female doctor in traditional clothing – most popular.
- Scores for women were higher than men.
- Older patients gave higher scores to both genders in the white coat.
- 64% of patients thought the way their doctor dressed was important.
McKinlay
- Investigate the perceived and actual comprehension of medical terms in lower working-class families.
- Researchers spent a month around doctors in gynaecology wards and collected 57 words.
- Doctors crossed off words that they don’t use often, resulting in 13 final words.
- In interviews, they were sounded out and used in a sentence.
- Participants asked to explain their understanding, which was recorded and reviewed by 2 doctors for accuracy.
- 18 other doctors were given the words and asked if they expect the lower class to understand.
- Compared the understanding of Under-Utilisers and Utilisers. Results:
- Utilisers had a better understanding of words (11/13).
- Doctors underestimated mothers' understanding.
- The term “Breach” was understood by most mothers, but doctors assumed only 22% of patients would understand.
- There is a tendency for doctors to use jargon without the expectation of patients understanding.
Patients might disclose information inaccurately because:
- They are angry.
- Ignore the doctor's requests.
- Insist on false medication.
Robinson and West
- Patients give more information to computerized interviews rather than questionnaires.
- Both methods gave more info than speaking face-to-face with a doctor.
False Positive / Type 1
-
Patient is healthy, diagnosed as sick.
False Negative / Type 2
-
Patient is sick, diagnosed as healthy.
Cooke and Colver
-
Investigated how patients with skin cancer would like to receive a diagnosis.
- Can be read anytime.
- No need to go to the hospital.
- Takes longer to be typed and sent.
- Not personal.
- Can't ask questions. Telephone:
- Quick.
- No need to go to the hospital.
- Can be done from home.
- Can be difficult to have a conversation.
- May not be available during the time of the call. Face to Face:
- More personal.
- Can ask questions.
- Can have a relative alongside.
- Need to go to the hospital. 52% of patients preferred a letter over face-to-face.
Letter:
Schofield
-
Wanted to evaluate the best way of breaking news to a cancer patient.
- Sent a questionnaire to patients 4 months after skin cancer diagnosis.
- No differences in satisfaction or depression between diagnosis by phone or face-to-face.
- Higher satisfaction when patients were prepared for diagnosis.
- Higher satisfaction when the word "cancer" was used, and when information was presented clearly.
Safer et al.
Munchausen Syndrome & Malingering
-
Appraisal Delay-
- Experience of the symptom.
- Observing for change.
- Emotional reaction to the symptom.
- Imagined consequence.
- Emotional factors.
- Beliefs about illness and medical services.
- Demographic and situational factors.
- 4 total clinics, 93 patients, and a 45-minute questionnaire and interview.
- Wide range of age and ethnicity, slightly more females than males.
- Interview designed to measure all types of delay and total time for each stage.
- Questionnaire had a mix of open and closed questions, used Likert-type scales.
The time taken to judge a symptom as an illness. These factors can increase this delay-
Results:
No correlation between the length of each delay stage.
Mean total delay was 57 days.
Most significant variable was “change in life unrelated to medical condition” such as marriage or divorce.
Those with this variable reported significantly later.
If the symptom was painful, the patient would report much sooner.
If the patient read about their symptom, they reported much later.
Under 45-year-olds would report sooner, over 45 delayed.
- Perceived Severity: Based on how serious the patient thinks the consequence might be.
- Perceived Susceptibility: Based on if the patient feels if they’re at risk.
- Perceived Benefit: Based on if the patient thinks the change will benefit them.
- Perceived Barriers: Based on if there are any barriers such as expenses, effort, discomfort, etc.
- Cues to Action: External events that could trigger a patient to take action.
- Self-Efficacy: A person’s belief in their ability to make a health-based change.
-
Munchausen Syndrome: Mental disorder where one pretends to be unwell. They hurt themselves.
Malingering: Somebody pretends to be unwell with an incentive, such as getting out of jail.
- Case Study
- 22-year-old female.
- Suffered from immune deficiency.
- Suffered from Amenorrhea (no periods) at age 17.
- Developed deep vein thrombosis.
- Developed swelling on both sides of the groin.
- Lumps developed in breasts that could not be explained.
- Led to suspicion of Munchausen syndrome.
- Patient underwent psychotherapy.
- Nurse found evidence suggesting the patient caused abscesses herself.